What are Venous Thromboembolism, Deep Vein Thrombosis, and Pulmonary Embolism?
Venous thromboembolism (VTE) comprises both Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE). VTE occurs on a spectrum of severity, from fatal PE to asymptomatic distal DVT, and not all types of DVT are equally likely to lead to PE.
DVT occurs when a blood clot forms in a deep vein, such as in a person’s lower leg, thigh, pelvis, or arm. It is important to note that DVT does not cause heart attack or stroke because of its location in a vein as opposed to an artery. A blood clot in an artery, typically in the heart or brain, is referred to as arterial thrombosis, which can lead to heart attack or stroke. DVT can, however, lead to pulmonary embolism, which is a medical emergency. PE occurs when a blood clot blocks blood flow to an artery in the lung. Often, the blood clot starts out in a vein in another part of the body, usually a deep vein in the leg, and travels to the lung.
What is the Healthcare Burden of Venous Thromboembolism?
Venous thromboembolism—including both DVT and PE—affects nearly 10 million people each year worldwide.1 While there are certain risk factors that can provoke DVT or PE, such as major surgery and cancer, most incidents involve patients without those risk factors. VTE is a serious global health burden, with high associated mortality, morbidity, and economic impact. VTE occurs on a spectrum of severity, from fatal PE to asymptomatic distal DVT, and not all types of DVT are equally likely to lead to PE.2
- The one-year case fatality rate of definite or probable VTE is estimated to be about 23%.3
- Risk for VTE increases with age. For patients over age 70, the incidence rate is between 2 and 7 in 1000, and for patients over age 80, the incidence rate is between 3 and 12 in 1000.3
- The incidence of VTE is higher in high-income countries than in low-income countries.2
Diagnostic Challenges with Diagnosing DVT and PE
In the last 30 years, there has been significant progress in developing and validating structured protocols to reliably assess a patient’s risk for VTE. These protocols combine patient characteristics, context, and predictive biomarkers with the aim of predicting risk for VTE and implementing preventive measures. However, when clinicians use diagnostic tests in populations with only low to moderate incidence of VTE, the positive predictive value is around 60%, and false positives are common.2 Because of the challenges with positive prediction of VTE, negative prediction (exclusion) is extremely important.
Thrombosis and Coagulation - Our Diagnostic Offer
Accessing information one single minute sooner can increase the probability that a life can be saved. In the case of VTE, rapid diagnosis is essential to ensure timely and appropriate treatment, reduce the risk of complications, and ultimately improve patient outcomes and quality of life. VIDAS® D-Dimer Exclusion™ II is indicated for use in conjunction with a clinical pretest probability assessment model to exclude deep vein thrombosis (DVT) and pulmonary embolism (PE) disease in outpatients suspected of DVT or PE. The combined use of clinical prediction rules and D-dimer testing as first screen allows rapid identification of patients who do not require imaging and in whom anticoagulant treatment can be safely withheld. In addition to this valuable biomarker, bioMérieux also offers validated result interpretation algorithms and clinical decision trees to support accurate and reliable biomarker usage.
Disclaimer: Product availability varies by country. Please consult your local bioMérieux representative for product availability in your country
-
VIDAS® D-DIMER EXCLUSION™ II
Safe Exclusion of Venous Thromboembolism
VIDAS® D-Dimer Exclusion™ II is a highly-sensitive automated D-Dimer assay. Used in conjunction with assessment of clinical pretest probability, it allows safe exclusion of deep vein thrombosis (DVT) and pulmonary embolism (PE) in both low and intermediate suspected outpatient risk groups in just 20 minutes.
-
MYACUTECASE™ Mobile App
All the information you need for confident clinical decision- making with the VIDAS® Emergency & Critical Care assays
Designed for healthcare professionals, MYACUTECASE™ is a first-of-its-kind app. Used in conjunction with clinical assessment and other laboratory findings, it provides comprehensive biomarker information and useful tools for:
-
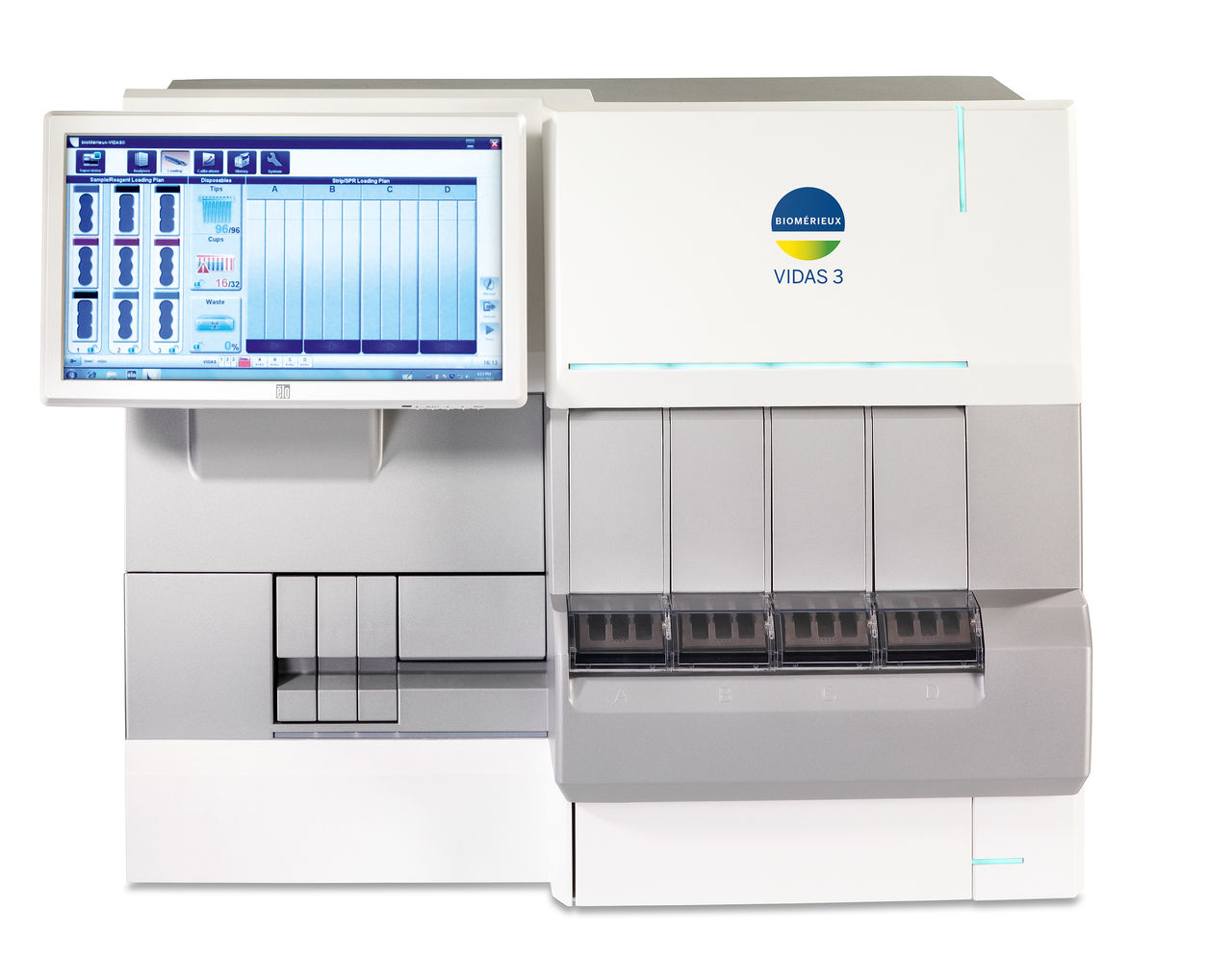
VIDAS® 3
Trusted. Robust. Innovative.
With its advanced immunoassay technology and optimized testing protocols, the fully automated VIDAS® 3 benchtop immunoanalyzer empowers your lab with confidence, offering the precise results you need, when you need them.
-
VIDAS® KUBE™
Stackable benchtop automated immunoassay solution
VIDAS® KUBE™ is designed to preserve everything labs appreciate about the VIDAS® Solution combined with advanced technology. VIDAS® KUBE™ is a truly flexible, cost-effective automated immunoassay solution providing fast results in complete confidence.
Useful Resources on Thrombosis and Coagulation
Contact Us for Information on Our Thrombosis and Coagulation Diagnostic Solutions
Contact Us
References
1. Khan F, Tritschler T, Kahn SR, Rodger MA. Venous thromboembolism. The Lancet. 2021;398(10294):64-77. doi:https://doi.org/10.1016/s0140-6736(20)32658-1
2. Nicholson M, Chan N, Bhagirath V, Ginsberg J. Prevention of Venous Thromboembolism in 2020 and Beyond. Journal of Clinical Medicine. 2020;9(8):2467. doi:https://doi.org/10.3390/jcm9082467
3. McCormack T, Harrisingh MC, Horner D, Bewley S. Venous thromboembolism in adults: summary of updated NICE guidance on diagnosis, management, and thrombophilia testing. BMJ. Published online May 19, 2020:369:m1565. doi:https://doi.org/10.1136/bmj.m1565